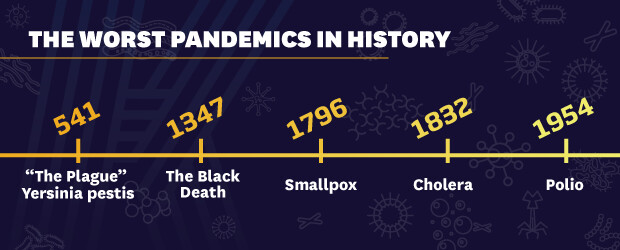
As COVID-19 numbers continue to increase, we can find encouragement by looking at some of the pandemics that preceded this one. Their numbers were staggering and the human responses to them not always productive, but there is hope in the repeated triumph of innovation and science over disease. As reassurance that we’ll conquer COVID, too, take a look at five of the worst pandemics in history—and developments that helped to end them.
MULTIPLE PLAGUES FROM A SINGLE BACTERIUM
Three of the deadliest pandemics in recorded history were caused by the bacterium Yersinia pestis—a lethal infection otherwise known as the plague.
The Plague of Justinian arrived in Constantinople (modern-day Istanbul), the capital of the Byzantine Empire, in the year 541. Having recently conquered Egypt, Emperor Justinian required tribute payments of grain. The plague came over the Mediterranean Sea in tribute ships, where infected fleas made the journey on black rats eating the grain. It decimated Constantinople and raged across Europe, Asia, North Africa and Arabia, killing an estimated 30 to 50 million people—perhaps half of the world’s population.1
How Did It End?
Other than trying to avoid those who were sick, people had no real understanding of how to fight disease. Historians speculate that the plague ended because the majority of people in a pandemic somehow survive, and survivors have immunity.1
THE BLACK DEATH AND THE IMPLEMENTATION OF QUARANTINE
When the plague returned 800 years later, it was known as The Black Death. It swept through Europe in 1347, claiming an astounding 200 million lives in four years.1
How Did It End?
Although there was no exact understanding of contagion, it was generally understood to be related to proximity between people. This led officials in the Venetian-controlled port city of Ragusa to keep newly arrived sailors in isolation until they could prove they weren’t sick. At first, they were held on their ships for 30 (trenta, in Italian) days, which became known in Venetian law as a trentino. Over time, authorities increased the enforced isolation to 40 (quaranta) days, or a quarantino, providing the origin of the word ‘quarantine’ and the start of its practice in the Western world.1
SMALLPOX AND A VACCINE
Smallpox was endemic to Europe, Asia and Arabia for centuries. Caused by the variola virus and highly contagious, it caused fever and a progressive, disfiguring skin rash. Three out of 10 people infected with it died. Many survivors were left blind or with permanent scars, often on their faces.2
When the first European explorers came to the Americas in the 15th century, smallpox came with them, to devastating result. The indigenous peoples of modern-day Mexico and the United States had no natural immunity to it, and the virus killed them by the tens of millions. Over a century, 90-95% of the indigenous population was wiped out. Mexico’s population dropped from 11 million to one million.1
How Did It End?
In 1796, British physician Edward Jenner found that milkmaids infected with cowpox, a milder virus, seemed immune to smallpox. He inoculated his gardener's eight-year-old son, James Phipps, with cowpox and exposed him to the smallpox virus. Despite several exposures, James did not develop smallpox.3 As a result of these tests and Jenner’s work over several decades, smallpox became the first virus epidemic ended by a vaccine.2
In 1967, the World Health Organization (WHO) launched a worldwide immunization program to eradicate smallpox. The last naturally occurring case was reported in 1977, and the WHO declared the virus eradicated in 1980.3
CHOLERA AND ADVANCES IN EPIDEMIOLOGY
Four major outbreaks of cholera between 1832 and 1866 ravaged London, killing tens of thousands of people. Then called ‘Asiatic cholera,’ the disease came to Europe from south-central Asia. Symptoms included stomach cramps, diarrhea, vomiting, severe pain in the limbs and severe dehydration that, untreated, could prove fatal within hours of occurring.4
The first identified, reported case of cholera in Britain was in October 1831, William Sproat, a keelman from Sunderland died three days after falling sick. On reaching London in 1832, it spread with terrifying speed. There was no known cure.4
Common belief held that cholera was airborne, transmitted via poisonous vapors (called ‘miasma’) from rotting organic matter. As many who suffered lived in overcrowded, polluted slums, this theory was widely accepted.4
In fact, cholera is produced by the bacterium vibrio cholera and transmitted via contaminated water sources. London’s population growth had far outpaced its infrastructure growth, and the city had no effective sewage system. This permitted raw sewage to contaminate the drinking water, the main source of which was the Thames river. As the river became increasingly polluted, the disease spread unabated.4
For decades, the government repeatedly enacted legislation to clean up the city, but each time, the suggested remedy was effectively to empty cesspools and raw sewage pits into the Thames.4
How Did It End?
Having argued in 1849 that cholera spread through ingesting contaminated water, Dr. John Snow was able to prove it in 1854. That August, an outbreak in London’s overcrowded Soho district killed more than 500 people in 10 days. By using a geographical grid to chart deaths from the outbreak and investigating each case to determine access to water from the Broad Street pump, he identified it as the outbreak’s source, and successfully arranged to have the pump disabled.4><s/up>
Although his findings were not immediately accepted, they influenced changes in public health and the construction of improved sanitation facilities.5 Today, John Snow is considered an essential link in the chain leading to modern-day epidemiology. His practices of placing cholera cases on a geographical grid and comparing incidence according to sources of household water supply were groundbreaking innovations in the development of the epidemiological approach.6
POLIO AND GLOBAL ERADICATION
In the early 20th century, polio was one of the most feared diseases in industrialized countries, paralyzing hundreds of thousands of children every year.7
The common name for poliomyelitis,8 polio is highly contagious, with symptoms including sore throat, fever, fatigue, headache, a stiff neck and stomachache.9 It’s caused by one of three types of poliovirus (members of the Enterovirus genus) which spread through interpersonal contact, nasal and oral secretions, and contact with contaminated feces. The virus enters the body through the mouth and multiplies through the digestive tract. In about 98% of cases, polio is a mild illness. In paralytic polio, however, the virus leaves the digestive tract, enters the bloodstream and attacks nerve cells. In severe cases, the throat and chest may be paralyzed and, without artificial breathing support, the patient dies.
Polio reached epidemic proportions in countries with relatively high standards of living.8 It struck in the warm months, which led to a mistaken belief in this country that it was caused by flies. In the years following World War II, Americans doused their neighborhoods, homes and children with the highly toxic pesticide DDT in the hope of eliminating polio, but more cases struck each season, peaking at 52,000 in 1952.9
How Did It End?
In 1947, epidemiologist Dr. Jonas Salk began to develop techniques to wipe out paralytic poliomyelitis. Contrary to his era’s prevailing scientific opinion, he believed that his vaccine, composed of “killed” polio virus, could immunize without infecting the patient. He administered it to volunteers who had not had polio, including himself, his lab scientist, his wife and their children. All developed anti-polio antibodies without negative reactions to the vaccine.10
In 1954, thanks to Salk’s innovation, national testing began on one million children, ages six to nine, who became known as the Polio Pioneers. On April 12, 1955, the vaccine was announced to be safe and effective. In the two years before it was widely available, the average number of polio cases in the U.S. was more than 45,000. By 1962, that number had dropped to 910.10
There is still no cure for polio. As the result of the global effort to eradicate it through vaccination, cases have decreased by over 99% since 1988, from an estimate of more than 350,000 cases to 22 reported cases in 2017. Today, only Pakistan, Afghanistan and Nigeria have experienced continuing transmission of the disease. Eradication efforts continue because even a single case of infection prolongs the risk of transmission.11
Salk neither patented the vaccine nor earned any money from his discovery, preferring that it be distributed as widely as possible. He founded the Salk Institute for Biological Studies in 1963 and spent his last years searching for a vaccine against AIDS. He died at 80 on June 23, 1995. His life’s philosophy is memorialized at the Institute in his own words:
“Hope lies in dreams, in imagination and in the courage of those who dare to make dreams into reality." 10
PUT YOUR COURAGE AND IMAGINATION TO WORK.
In 2021, more than at any time in living memory, there is a global need for health specialists equipped with new methods and technology to solve immense problems. Become a leader in a field that affects—and can save—millions of lives. Study with the experts at Kent State and earn your online Master of Public Health in Health Policy and Management, Social and Behavioral Sciences or Epidemiology, or your online Master of Science in Clinical Epidemiology.
- Retrieved on February 5, 2021 from history.com/news/pandemics-end-plague-cholera-black-death-smallpox
- Retrieved on February 5, 2021 from niaid.nih.gov/diseases-conditions/smallpox
- Retrieved on February 5, 2021 from jenner.ac.uk/about/edward-jenner
- Retrieved on February 5, 2021 from thegazette.co.uk/all-notices/content/100519
- Retrieved on February 5, 2021 from rcseng.ac.uk/library-and-publications/library/blog/mapping-disease-john-snow-and-cholera/
- Retrieved on February 5, 2021 from ncbi.nlm.nih.gov/pmc/articles/PMC3730273/
- Retrieved on February 5, 2021 from polioeradication.org/polio-today/history-of-polio/
- Retrieved on February 5, 2021 from historyofvaccines.org/timeline/polio
- Retrieved on February 5, 2021 from history.com/news/polio-fear-post-wwii-era
- Retrieved on February 5, 2021 from salk.edu/about/history-of-salk/jonas-salk/
- Retrieved on February 5, 2021 from who.int/news-room/q-a-detail/does-polio-still-exist-is-it-curabl