College of Public Health
Kent State University’s College of Public Health is at the forefront of addressing critical health issues and training the next generation of public health professionals. Faculty members actively engage in impactful research, such as the Greater Cleveland LGBTQ+ Community Needs Assessment, and tackle global challenges like food deserts and public healthcare economics. With programs designed to prepare students for diverse careers in public health, the College offers advanced learning opportunities in areas like epidemiology, public health interventions, and healthcare disparities. Through innovative teaching and meaningful research, Kent State’s College of Public Health continues to shape the future of community health and well-being.
Related Blog Posts
More than 60,000 Cleveland residents identify as lesbian, gay, bisexual or transgender.1 To better understand these residents’ needs, the Kent State University College of Public Health (CPH) launched the Greater Cleveland LGBTQ+ Community Needs Assessment project in March. The LGBT Center of Greater Cleveland serves as the primary community partner, and the Cleveland Foundation is providing financial support.
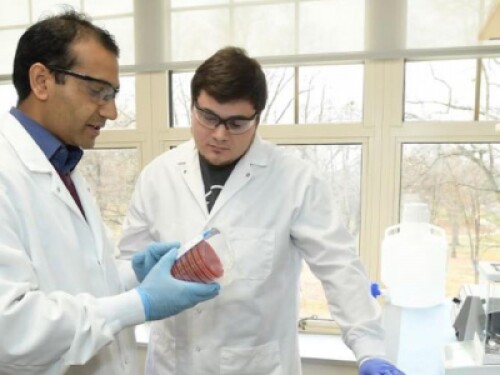
Kent State University’s College of Public Health (COPH) faculty are engaged in community-based, relevant research and public health programs, continuing the tradition of excellence and service that began when Kent State was founded as a public research university in 1910. In this post, we introduce you to three of the COPH professors who are actively engaged with their communities and their students, and with advancing knowledge in their areas of expertise.
I am a professor and the associate dean for Research and Global Affairs. I teach undergraduate, master, and doctoral-level courses. Most courses I teach focus on applying theory to developing, implementing, and evaluating community-based public health programs. I direct doctoral dissertations and advise MPH students. In my role as associate dean, I facilitate the research enterprise in the College, including pre and post-award activities, research compliance, and serve on university research-related committees. In addition, I develop research projects with other institutions abroad, faculty and student exchanges, and promote faculty and student research.
Public health careers are broad and varied, and for those who are passionate about changing lives for the better, they present an immense opportunity to fill growing needs in the field. A Master of Public Health degree demonstrates your pursuit of advanced knowledge, desire to lead, and a set of professional skills needed to succeed in a variety of healthcare careers and public health roles.
Quality Matters™ (QM) is a nationally recognized, faculty-centric non-profit that looks at how educational institutions measure and guarantee the quality of a course, specifically the course design. Quality is measured through both a rubric and a rigorous peer-review process.
Public health experts have never been more important than they are in the world today. From cancer to Ebola to COVID-19, major health events affect us all. As globalization, climate disasters and economic and social disruptions expand, we need trained professionals to help mitigate those threats. To meet health needs, public health professionals continue to serve and protect through research, policymaking and administration in the field of infectious disease preparedness and prevention. Specialists in the field of epidemiology are responsible for some of today’s most important public health research and data analysis.
As 2021 comes to a close, we’re taking a look at some of the top public health problems that faced the world in the past year. While some are more obvious than others, they all tie together to form a picture of the biggest challenges facing humanity today and give us a clue as to what to expect in the future.
The Centers for Disease Control and Prevention (CDC) define epidemiology as the study of the distribution and determinants of health-related states and events in specified populations.1 To complete this study of “health-related states and events”, scientists use a tool called the epidemiologic triangle, or the epidemiologic triad.
The Bureau of Labor Statistics estimates that healthcare positions will grow by 4.6 million by the year 2029 and that six out of the 10 fastest-growing occupations will be related to healthcare.1 Given recent global health events, it stands to reason that jobs in public health would be growing as well.
Epidemiologists are public health workers who investigate patterns and causes of disease and injury.
Join Kent State University in celebrating World Health Day on April 7, 2021, to build a fairer, healthier world.
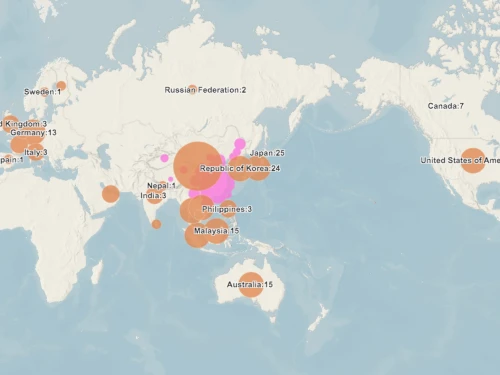
Discover how mapping coronavirus transmission can prevent outbreaks in countries outside of mainland China.
Ken Slenkovich is the assistant dean of Kent State University’s College of Public Health and program director for the school’s online Master of Public Health program. Leveraging his diverse experience as a public health professional, with research endeavors that have focused on the operations of local health departments and community health needs assessment methodologies, Asst. Dean Slenkovich has helped to elevate and enrich our nationally celebrated online MPH program, even authoring an award-winning course for the program.1
Public health careers appeal to different people for different reasons, just as certain universities make more sense for certain individuals. The university you choose should be a conduit through which you can achieve your aspirations, and there are many factors to consider in the selection process. For some the most important of these may be prestige, while others may weigh connections or affordability more heavily.
Of the nearly 323 million individuals who live in the United States, almost seven percent make their home in a food desert. That means more than 23 million Americans, including millions of children, are without consistent or easy access to fresh, nutrient-dense meals and groceries.1 It’s an alarming trend that has accelerated with other changes in modern cities, including suburbanization, growing socioeconomic inequality and increasingly inadequate public transportation. Some of the traumatic effects these food deserts have on public health include growing rates of chronic disease and obesity.
If “public health” refers to caring for the collective health of a population, then “public health economics” is the science of how a society takes on and manages this responsibility with limited resources. Public health policy is broad: While some of it does focus directly on healthcare, other areas as disparate as environmental protection, individual habit change and infectious disease control all contribute to the economics of public health.1 Studies indicate that there are economic benefits to preventing disease, not just for sick individuals, but for society at large.
Evidence-based public health interventions have saved millions of lives since 1854, when Dr. John Snow first identified a public water well as the source of a major cholera outbreak in London. In the decades since, public health interventions have been instrumental in improving the health and well-being of people in large and small communities.1
Throughout the mid-19th century, clinicians noted the impact of socio-environmental factors on healthcare. From unusually high incidences of breast cancer in Italian nuns to cancers that only seemed to affect chimney sweeps in Great Britain, medical literature of the period carefully traced the connections between cultural background and wellness. This led some physicians to theorize that disease was strongly related to societal dysfunction and inequality, and that improving schools and working conditions could help to alleviate disparities in mortality across social classes.
It can be easy to take for granted the comforts that most of us have in our homes. Indoor plumbing, running water, heat, a safe place to sleep, food—even the people fortunate enough to enjoy these amenities will periodically fall ill. Yet they can maintain their cleanliness, get adequate rest and most likely have access to reputable health care. Now, take all of that away. Suddenly, an alarming range of bodily and psychological impediments can arise.