Kent State University College of Public Health Blog
To determine if public health has a place in the social sciences, we should first clarify what constitutes a social science. From there, we can easily see whether one discipline fits within the other, and we’ll have our answer. Nice and simple.
With the urgency of the coronavirus pandemic, the climate crisis and other global health challenges on the horizon, there is perhaps no more important field today than public health.
Discover the real differences between community health and public health. Learn how each impacts healthcare, careers, and your future in the field.
Understand the core public health services that drive real change. Discover how each function supports careers in health equity, policy, and prevention.
This post explores the difference between an MPH and an MSPH, as well as which career paths are available after completing each degree. Compare curricula, job prospects, and more!
Explore the Master's in Public Health requirements, from academic prerequisites to application materials. Prepare for your MPH journey today!
Uncover the wide range of career possibilities for MPH graduates. Learn about traditional and emerging roles to find your ideal path in public health.
Explore the future of public health in 2025 and beyond. Discover emerging trends, career growth opportunities, and technological innovations!
Explore the path to a rewarding career in clinical research. Get expert tips on education, experience, and job hunting in this complete guide.
Explore the fundamentals of clinical research. From study designs to ethical considerations, gain insights into this crucial field of healthcare.
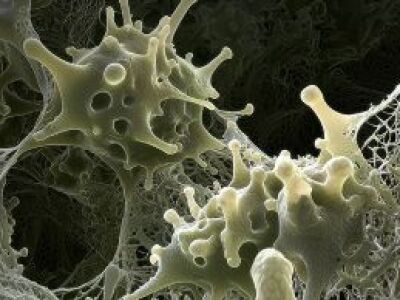
Explore the world of epidemiology, where disease detectives work to protect public health. Learn how they track, prevent, and combat outbreaks.
Sometimes people wonder, "What is the role of epidemiology in public health?" Like public health, epidemiology focuses on macro-scale health trends and uses data to determine how to improve health outcomes for populations. This post explores the way the fields of epidemiology and public health support and reinforce one another.
Explore the epidemiological triangle in-depth and cover how you can apply it in your epidemiology career.
Discover the top clinical research organizations driving medical innovation. Learn how these top CROs are shaping the future of healthcare.
Evidence-based public health interventions have saved millions of lives since 1854, when Dr. John Snow first identified a public water well as the source of a major cholera outbreak in London. In the decades since, public health interventions have been instrumental in improving the health and well-being of people in large and small communities.
Explore how public health drives disease prevention. From community strategies to global initiatives, learn about the impact of preventive measures.
Learn how mental health advocacy is revolutionizing public health approaches. Get insights on successful programs, policy implementation, and more.
Discover vital public health emergency preparedness guidelines to protect your community and learn tips for effective response planning.
Discover effective strategies for implementing community-based health interventions, including health education, outreach programs, and public health education initiatives.
Explore comprehensive public health strategies, including community health improvement, disease prevention, and effective public health programs for community wellness.